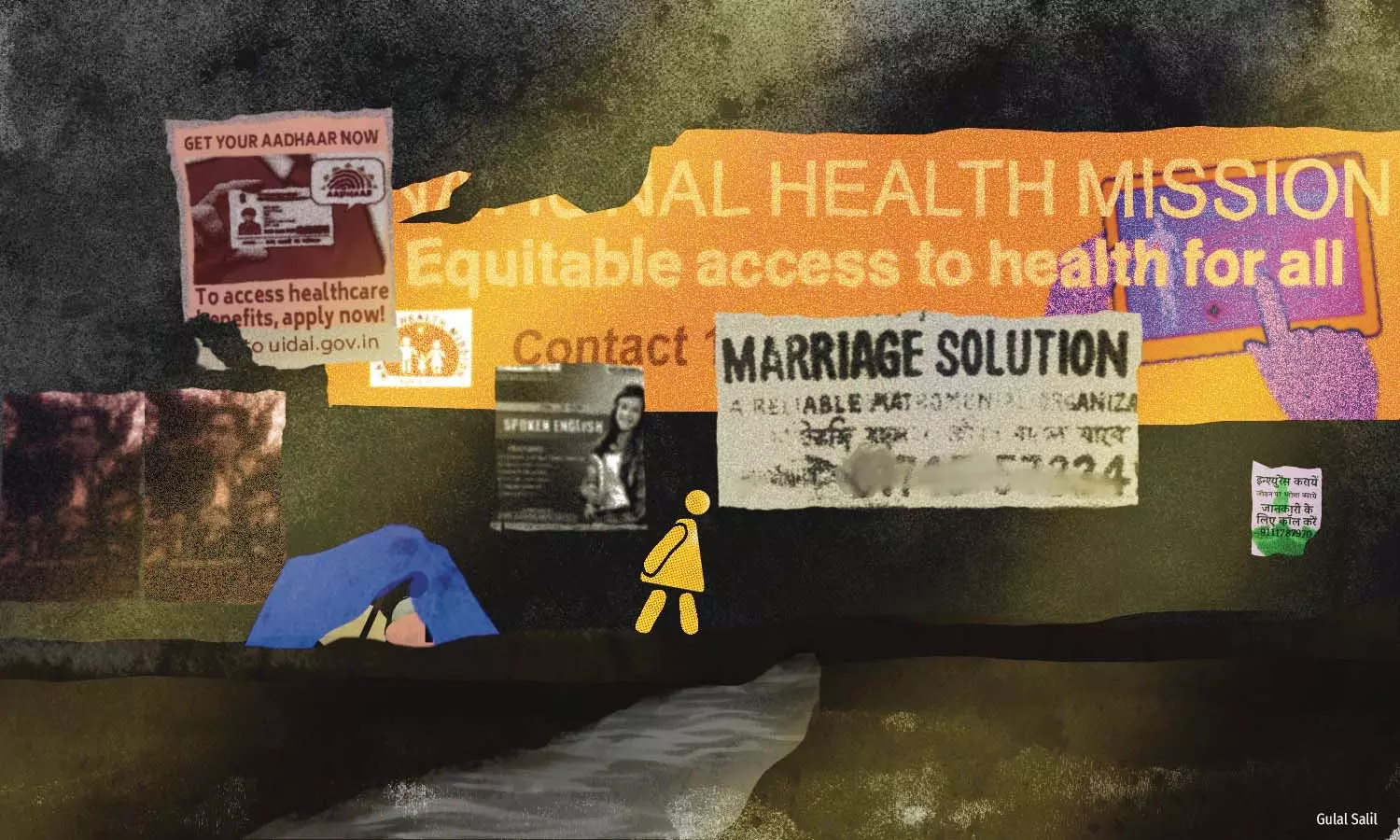
How Rohingya Refugees Are Impacted By Limited Access To Healthcare
Rohingya refugees are able to access basic healthcare, but they find it difficult to access specialised care, often leading to high out of pocket expenditure and debt
Bengaluru, Delhi and Nuh, Haryana: Wasim* folds a part of his chequered lungi above his right knee and sits with his right leg outstretched on the floor of his neighbour's makeshift tent. He swats at a fly trying to perch on the open wounds on his knee and toe, on this August morning in Bengaluru.
Wasim was knocked out cold for several minutes after being hit by a passing vehicle during his daily work as a waste picker. He has been dealing with unbearable pain for nearly a week due to his injuries. Inadequate medication and treatment made it worse.
As a Rohingya refugee, the 35-year-old has endured violence and a life of uncertainty for over a decade. He survived a bullet to his leg, a constant reminder of the persecution his community faces in the Rakhine state of western Myanmar, and the reason he fled to India. But this latest injury has him worried.
He made three trips to get treated--twice to a private facility and once to the government hospital around 5 km away from the settlement. “It cost me Rs 800, which I had borrowed, to dress my wound and get some medicines at a private facility. But when I went to the government hospital they asked me to do an X-ray privately because the facility there was crowded,” said Wasim. “When I visited the private health facility again, they gave me some tablets. I did not have money, so I did not bother to check about the X-ray costs.”
Unable to work, Wasim worries about how to feed his family of eight that depends on his monthly earnings of Rs 8,000.
More than 2,000 km north of Bengaluru, in Haryana’s Nuh, one of the least developed districts in India, Nuzrat* cradles her four-year-old daughter, who is on intravenous therapy due to high fever. The last year has been traumatic for Nuzrat. Her husband, a diabetic who was paralysed, had passed away. In early 2023, her eldest son, only 17, died due to tuberculosis-related complications. The eldest of her surviving children, a son aged 15, stopped working as a waste picker after he was threatened by locals when he demanded wages for four days of work.
Nuzrat has no job; she has sold most of her jewellery to finance the various medical treatments and is now in debt to the tune of Rs 70,000. She struggles to manage her household, which includes five children. “I want to move to Hyderabad where women are able to do some work to earn,” said Nuzrat.
In the first of our two-part series based on reporting in Bengaluru, Delhi and Nuh, IndiaSpend found that Rohingya in India are able to access basic healthcare through United Nations High Commissioner for Refugees (UNHCR) cards and NGO support at government hospitals. However, they find it difficult to access and sustain specialised care or emergency treatment, for which they have to mostly pay out of pocket.
Any adverse health issue--which many are susceptible to due to their unsanitary living conditions caused by lack of proper housing, nutritious food and clean water, poor sanitation and unhealthy work conditions--aggravates their vulnerability. Language barriers, low health-seeking behaviour and socio-economic circumstances add to their woes, say experts.
How many Rohingya are in India?
Most of the 1.3 million displaced stateless people worldwide are Rohingya, either internally displaced in Myanmar, or refugees mostly in neighbouring countries. The 1982 Burma citizenship law excluded Rohingya from the list of 135 officially recognised ethnic groups, rendering them stateless. Predominantly Muslim, Rohingya people are reported to be the largest stateless population and “the most persecuted minority in the world”. The lack of citizenship or legal identity in Myanmar impacts their access to basic rights and protection, forcing them to flee violence and “ethnic cleansing”.
India hosts more than 212,000 refugees and asylum seekers. It is reported to have 22,110 Rohingya refugees and asylum seekers, which was 2% of the nearly 1.1 million Rohingya refugees and asylum seekers outside Myanmar, as reported by the UNHCR. Many live in small informal settlements in Delhi, Jammu, Bengaluru, Hyderabad, Mewat and other parts of the country.
According to UNHCR data, less than one in three refugees and asylum seekers from Myanmar in India were Rohingya, which is much lower than the number of Rohingya in other countries bordering Myanmar. Nearly all Myanmar refugees in Bangladesh were reported to be Rohingya, while the corresponding numbers were 67% in Malaysia and 97% in Indonesia.
We filed a right-to-information (RTI) request with the Union home ministry seeking the exact number of Rohingya in India. The ministry forwarded it to the Intelligence Bureau, which did not provide the data, claiming that such information was exempt under Chapter VI, section 24 (1) and the Second Schedule of the RTI Act. These sections deal with exemptions provided to intelligence and security organisations, and limit the rights available under the Act to access information. The Foreigner’s division did not have the information.
In the ongoing Supreme Court hearing of petitions challenging the constitutional validity of Section 6A Of The Citizenship Act 1955 in the Assam Accord, the government said that it is not possible to estimate “illegal immigration” in India. In an April 2022 RTI response, the home ministry had told IndiaSpend that “since illegal migrants including Rohingya enter into the country in clandestine and surreptitious manner, accurate data regarding the number of such migrants living in the country is not centrally available”.
Documentation and health
Nuzrat visited Safdarjung government hospital in Delhi, around 70 km away from her refugee camp in Nuh, to find treatment for her son. She found the medicines and injections, which she had to buy separately, expensive. Since there was no access to proper treatment in Nuh, she had no choice. “I had some gold which I sold; I got Rs 35,000 worth of financial support from the community, and Rs 19,000 from locals.”
There are two hospitals at present catering to most of the refugees in Mewat--one in Nalhar, the other being Nuh Medical College, said a report by Human Rights Law Network based on visits to Rohingya camps in Mewat, Delhi and Faridabad in 2017.
“... in both places there are only a few medicines available and in the former, Rohingyas who go there are more often than not transferred to Delhi,” the report said.
Due to their status as refugees, and particularly the government’s categorisation of Rohingya as “illegal migrants”, they are not issued Aadhaar cards, the de facto identity proof to access welfare schemes in India.
Rohingya refugees told IndiaSpend that they were generally able to access basic health services at the government hospitals even without Aadhaar. The UNHCR card, which is usually the only official documentation most Rohingya possess, suffices.
This however does not mean that all health services are accessible to them.
A report by The Azadi Project and Refugees International showed that even though “92% of Rohingya refugees said that they have access to healthcare services, most of them cannot access specialised treatment or care”.
On October 27, the Unique Identification Authority of India (UIDAI), which is in charge of issuing Aadhaar, responded to an IndiaSpend RTI query, saying that a “Resident Foreigner (nationals of Nepal/Bhutan)” is entitled to obtain an Aadhaar number if they satisfy the eligibility criteria and produce appropriate documentation”. A resident is defined as an individual who has resided in India for a period or periods amounting in all to 182 days or more in the 12 months immediately preceding the date of application.
Until 2017, the Rohingya community was granted Aadhaar cards in accordance with the prevailing regulations, which stipulated that individuals who had resided in the country for a duration exceeding 182 days were eligible to obtain it, said Fazal Abdali, a refugee rights lawyer.
On August 9, 2017, the Union government said that there were "around 40,000 Rohingyas living illegally in the country", and issued an advisory on the identification and monitoring of "illegal migrants” who have been specifically identified as “from Rakhine State, also known as Rohingya”.
“Following the government's declaration that the Rohingya population was deemed illegal, their access to Aadhaar became restricted. Also, Long Term Visas (LTVs) have not been granted to the Rohingya since August 2017,” Abdali said.
An LTV (for stay of more than 180 days)--which is not available to Rohingya refugees--is essential for refugees to gain access to various documents including Aadhaar, bank accounts, driver’s licence, or for buying property.
Due to this lack, Rohingya people are unable to take up any transportation jobs or legally acquire a vehicle for personal purposes, and without a bank account, they are essentially excluded from an increasingly ‘cashless’ digital economy that India is aiming to become, said a December 2020 analysis by researchers Anubhav Dutt Tiwari and Jessica Field.
“These restrictions are undermining Rohingya opportunities for self-support and increasing their dependence on humanitarian aid,” the analysis said.
Wasim, who has lived in Delhi for more than eight years, said that his father--who too was shot before they fled from Rakhine in 2014--got inadequate treatment for injuries in the refugee camp in Bangladesh.
The family then came to India. After months of tests at government hospitals in Delhi, his father was eventually diagnosed with cancer a few months before his death. Wasim was asked to take his father to a private hospital because treatment was not available at the government hospital. “Someone [at the hospital] also told us that we could go to Kerala where I could get help, but it was far, and expensive to travel to an unfamiliar place,” he said. His father died in 2017.
Rohingya refugees who suffered from noncommunicable diseases (NCDs) such as diabetes and blood pressure, tumours, or whose children were unwell or injured and required specialised treatment, said that they were unable to afford medical care without more financial support.
For example Rehana*, a Rohingya refugee, whose three-year-old son had severely burned his hand over a year ago in Bengaluru, feels guilty about the accident. Her husband, a waste picker who earns about Rs 10,000 a month, blames her for the child’s plight. “The hospital said it (treatment) will be difficult and cost around Rs 2 lakh. How will we afford it?”
Even during the Covid-19 pandemic in 2021, refugees had problems accessing vaccines. India's Covid-19 vaccine policy made all its adult citizens eligible, but made no mention of the undocumented immigrants and refugees who live and work here, IndiaSpend reported in May 2021.
During the peak of the pandemic, the community was vilified following media reports alleging that they had created coronavirus clusters in the country due to contact with members of the Islamic missionary group Tablighi Jamaat.
Outside the ambit of social protection
Major social protection schemes including health-related support exclude refugees.
The Union government’s Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PM-JAY) aims to provide a health cover of Rs 5 lakh per family per year for secondary and tertiary care hospitalisation to the bottom 40%--the poorest--of the Indian population.
The cost of health expenditure is high for citizens, which was a reason to launch PMJAY--so as to mitigate “catastrophic expenditure for hospitalisations”. In 2014, the last year for which data are available, the average cost of inpatient care per hospitalisation in India was Rs 26,475 in urban areas and Rs 16,676 in rural areas, IndiaSpend reported in March 2023.
PM-JAY beneficiaries are identified based on deprivation categories specified under the Socio-Economic Caste Census database for rural areas, and 11 occupational criteria for urban areas.
According to the provisions of PM-JAY, no one can be denied entitlements for lack of an Aadhaar card. But in 2018, UIDAI said in a tweet based on a news report that Aadhaar is mandatory if beneficiaries want to be treated for the second time. A 2023 Comptroller and Auditor General performance audit report of the scheme also mentions the compulsory requirement of Aadhaar-based identification for availing the scheme.
This suggests that Rohingya are excluded from the social protection despite many working as rag and waste pickers, which are occupational categories entitled to avail benefits.
Similarly, access to the centrally sponsored Janani Suraksha Yojana (JSY), which encourages institutional delivery and provides cash assistance with delivery and post-delivery care to women, is also not accessible. The online application mandates the furnishing of Aadhaar, which automatically excludes refugees including Rohingya.
IndiaSpend filed for information under RTI with the Ministry of Health and Family Welfare (MoHFW) and the Ministry of Home Affairs for data and information on health access for Rohingya, the need for Aadhaar cards to access medical care in government or private hospitals, health and social protection schemes that can be accessed by Rohingya, and the total number of Rohingya in India. The responses either did not specify if, and if so how, refugees can access healthcare services and documentation like Aadhaar, or said that the information was ‘nil’.
Union Govt’s RTI Responses Did Not Provide Refugee-Specific Information Various ministries and departments of the Union government responded to our RTI requests, but did not specify support for refugees or Rohingya in particular. The Ministry of Women and Child Development said Saksham Anaganwadi and Poshan 2.0 provide packages of six services to “all eligible beneficiaries”, which included children between 0-6 years, pregnant and lactating mothers. The maternal health division said that “irrespective of religion, caste, and state domicile,” schemes like Surakshit Matritiva Aashwasn, JSY, Janani Shishu Suraksha Karyakram, PM Surakshit Matritva Abhyan, High Risk Pregnancies and LaQshya were being implemented. The National Health Mission-2 division said public health and hospitals is a state subject, and all matters of strengthening health systems lies with the respective states. The All India Institute of Speech and Hearing (AIISH) in Mysore responded saying that all services are provided equally to patients and that Aadhaar and UID “is not compulsory to access services at AIISH, Mysore”. The All India Institute of Physical Therapy and Rehabilitation in Mumbai said that the information sought was “not available”, and that “there is no separate fund allocated nor is there any specific healthcare scheme for Rohingya refugees at the institute”. The child health division, in a September 4 response, said that any child enrolled in government or government-aided schools or anganwadis (childcare centres) are screened by Rashtriya Bal Swasthya Karyakram, the government’s child health screening and early intervention services. This was followed up by another response from the division on October 17, which said that all interventions to reduce child morbidity and mortality are being implemented universally in all states/UTs with a “focus on tribal and marginalised population without any discrimination on gender, caste and religion”. The health ministry’s various divisions like Non Communicable Diseases-1, e-health, public health, National AIDS Control Organisation (Care, Support and Treatment Division), and central Tuberculosis division said the information sought is not available and may be treated as “nil”. |
These official responses underline the challenges faced by stateless Rohingya in India--a situation that is similar in other countries to which they have fled. A May 2022 paper by Surendran Rajaratnam and Azlinda Azman in the International Journal of Environmental Research and Public Health found that in terms of financial barriers to access health services, Rohingya informants, 22 women, in Malaysia mentioned that they faced problems accessing hospitals because they could not afford the cost of the treatment and medicine charged.
Healthcare experts such as Aqsa Shaikh, a doctor and community medicine specialist who has treated Rohingya refugees in Delhi NCR, said that Rohingya are left out of the public health safety net and do not have access to Ayushman Bharat, which is a major Union government scheme.
“They do not have the necessary documents,” Shaikh said. “The state government provides primary health services through Mohalla clinics but cases which require admission through schemes like Delhi Arogya Kosh [financial support for health in Delhi government hospitals] does not cover them.”
This issue of not having Aadhaar has also affected non-health needs of refugees. Before Aadhaar became widely used in 2015, refugee women were getting cash support under the JSY, said Ravi Hemadri, Director, Development And Justice Initiative (DAJI), a non-profit promoting rights and access to justice for adivasis, refugees and migrant workers. “Since linking to Aadhaar [was made mandatory] this has stopped. Children do not get textbooks and uniforms and mid-day meals. Admissions are provisional due to this.”
In April 2017, the National Commission for Protection of Child Rights, on a complaint from DAJI, had categorically said that “no admission is to be denied to any child seeking admission in a government or government aided school in Haryana”.
NGOs provide health access and support
Due to the lack of a uniform refugee policy, presently, various UNHCR-supported NGOs implement schemes for refugees to assist the most vulnerable by covering their expenses and filling some gaps through volunteers, who liaison with hospital staff and inform them of refugees.
The refugees are able to access some medicines and reimburse bills for some medical procedures through NGOs, refugees in Delhi told IndiaSpend. But in case of an emergency, they tend to visit private hospitals that are near their settlements in the Kalindi Kunj area. Large government hospitals like Safdarjung and Ram Manohar Lohia are at least 30 minutes away, and have a long waiting time.
An NGO that did not want to be identified said that access to healthcare has been positive and doctors treat Rohingya refugees like any other patients, due to the active presence and involvement of various civil society organisations. But certain benefits such as JSY or birth control-related entitlements are not given due to lack of documentation like Aadhaar.
Some NGOs like DAJI are working, with the local health administration’s support, in Nuh to provide Rohingya refugees with better access to government health facilities so that lack of documentation is not a hurdle to access healthcare.
The UNHCR India told IndiaSpend in response to queries on healthcare and government social protection access that it appreciated the Union government's “unwavering support” towards refugees and asylum-seekers for providing healthcare access at par with citizens. Refugees and asylum seekers can access primary, secondary and tertiary government healthcare facilities, it said.
However, the response also mentioned that the absence of a government-issued legal identity [like Aadhaar] poses a challenge for refugees and asylum-seekers as it excludes them from the government's social protection programmes.
“This, in turn, necessitates them to cover the costs of medical tests, investigations, treatments, and medications that may not be readily available in government pharmacies.” UNHCR India, through its NGO partners, assists the “most vulnerable refugees” in covering these medical expenses, they said.
According to the UNHCR India review of 2022, 43,238 refugees overall were provided access to healthcare, including medical tests and treatment.
No refugee-asylum legislation
India does not have a legislation on refugees and asylum seekers, and is not a signatory to the 1951 UN Convention relating to the Status of Refugees and the 1967 Protocol. Therefore any persons crossing the borders into the country without permit are deemed to be “illegal migrants”, including Rohingya who “pose a threat to national security”, according to the Union government.
The Rohingya crisis was one of the reasons that prompted Shashi Tharoor, Member of Parliament from Thiruvananthapuram, to introduce a Private Member's bill in February 2022, seeking to provide a legal framework to protect refugees and asylum seekers, including access to the same healthcare services as Indian citizens.
As a democracy upholding human rights, India should have some policy to address refugee rights, said K.M Parivelan, associate professor, Centre for Statelessness and Refugee Studies, School of Law, Rights and Constitutional Governance, Tata Institute of Social Sciences, Mumbai.
The argument of volatile neighbourhood and economic challenges are diversionary. “We have an obligation. Rohingyas are persecuted in Myanmar which shows that they should be politically protected in India and voluntarily repatriated when it is safe for them to return,” Parivelan said.
The 2013 Jaffar Ulla petition pending in the Supreme Court was filed based on findings of health activists in 2012 that there was inadequate maternal healthcare, medical aid, nutrition and hygiene, among other issues, for Rohingya in Mewat and Delhi.
It was reported that the Union government submitted to the court that JSY benefits cannot be provided as they do not belong to Scheduled Castes and Tribes or to the below-poverty-line category.
In an August 2018 directive, the Supreme Court asked the Sub-Divisional Magistrate or the equivalent authority of District Mewat, Haryana that the concerned jurisdictional revenue magistrate be appointed as nodal officer to ensure proper availability of limited entitlements. The order also extended to Kanchan Kunj and Kalindi Kunj in Delhi, where Rohingya reside.
“The provision of emergency or specialised care from the government is currently lacking a systematic process, necessitating reliance on the assistance of NGOs for such services,” said Abdali, who is representing Jaffar Ulla before the Supreme Court.
IndiaSpend has written to senior officials in the MoHFW, Delhi health services, the commissioner of Faridabad Division, the deputy commissioner and district health officials of Nuh, and to the Karnataka health and family welfare services for their responses on healthcare access and support provided to Rohingya refugees. On October 20, IndiaSpend received a letter from the Faridabad division commissioner requesting Nuh’s deputy commissioner to share information based on the request. We will update the story when we receive a response.
Institutional deliveries
Wasim, who was recovering from his injuries, had not worked for over a month when IndiaSpend met him in late September. Since his accident in mid-August, he had incurred a debt of Rs 40,000, nearly five times his monthly earnings, and was desperate to return to work. His wife, Noor*, who along with him relocated from Jammu to Bengaluru in December 2022, delivered a child in October.
Five of his six children were delivered at home and at least three of his children have not been immunised, including his youngest born in October, he told IndiaSpend. He had gone to the hospital for immunisation of one of the children recently, but he was shuffled around and made to wait by the hospital staff. Fed up, he left.
When Noor was pregnant, she got one dose of vaccination in Jammu in February. Based on the details of the Union government’s mother and child protection card, a pregnant woman must at least have three antenatal checkups, take two tetanus toxoid injections, and take one tablet of iron folic acid a day for at least six months after the first trimester.
Most Rohingya women who spoke to IndiaSpend said that they got iron and calcium tablets, but scans like ultrasound, which cost Rs 100 at a government hospital in Bengaluru, and any other related support was not available consistently. At private hospitals and clinics, which many women utilise, scans incurred higher costs.
In Delhi and Nuh, Rohingya community members, preferably women, work as health support volunteers who help book appointments and speak to doctors and staff.
“During my pregnancy I went to the government hospital here [Bengaluru] twice, but they asked us for money and I have not done any scans,” she said. “Where do we have the money even if it is Rs 100?” The staff at the government dispensary was annoyed that she did not have a Thayi card (mother and child protection card in Karnataka). Noor bought medicines from a private dispensary.
“If women are able to have regular antenatal checks, complications can be managed, but if they only approach hospitals during delivery and not earlier, it will not ensure continuum of care,” said Sylvia Karpagam, a public health doctor and researcher who has conducted health camps with refugees and vulnerable communities. “Complications have to be picked up early. Government facilities do not necessarily cater to actively looking for vulnerabilities in such groups.”
Refugee children have access to immunisation and are unable to get supplementary nutrition as it is linked to Aadhaar card, said UNHCR India.
In a household earning around Rs 10,000, more than half is spent on food and groceries, leaving almost nothing as savings. Given they are excluded from the public distribution system, it limits their ability to access adequate and nutritious food, which affects the health of children and lactating mothers.
Fund crunch becomes a challenge while providing aid and support. With more than 47,000 asylum seekers and refugees registered with UNHCR India, only 28% of the financial requirement of $21.7 million (Rs 181 crore) for 2023 has been met. “UNHCR provides protection, solutions and assistance to those registered with us. However, as needs grow, our ability to respond to growing needs is severely threatened by limited funding,” said UNHCR India.
Health-seeking behaviour
Often, Rohingya women prefer to give birth at home, usually assisted by an older woman who is a birth attendant. A 2020 cross sectional study based on a rapid assessment of Rohingya refugees in Bangladesh’s Cox’s Bazar--the world’s largest refugee settlement--by Mohammaed Ridwanur Rahman and others showed poor health literacy and health status.
It said that overall, there was poor understanding regarding treatment of common illnesses such as diarrhoea, and that the majority (90%) of childbirths occurred at home, with only 4% occurring in the presence of a trained healthcare worker.
In Bengaluru, one attendant said that she had been asked by local health workers not to continue home deliveries in order to encourage institutional deliveries. Usually the children were immunised during hospital visits and given birth certificates if it was an institutional delivery, although visits by health workers were not systematic, refugees said.
The UNHCR provides Rs 6,000 for one institutional delivery in a government hospital. But, as we said earlier, lack of access to documentation makes refugees ineligible for the government schemes which provide ante- and postnatal financial assistance to women.
Culturally, Rohingya women prefer female doctors due to which they prefer home deliveries instead of institutional deliveries, said a doctor who did not want to be identified. “It would be useful if the government can train and licence individuals from the community to be link workers similar to ASHAs. This would help women deal with language barriers and access proper healthcare,” said the doctor.
While there has been improvement in the number of Rohingya women opting for institutional deliveries owing to the work of UNHCR and NGOs, for various reasons, including cultural norms, financial challenges, and discrimination, they mostly choose to give birth at home, said the report by The Azadi Project and Refugees International.
Experts working with Rohingya said that more can be done if there is political will. Community members and medical staff can be trained to provide health aid support and be more sensitive to refugee needs.
Wasim, meanwhile, was desperately trying to fix his damaged rickshaw, which would cost him more than Rs 1,000, an amount he did not have. “My injuries are healing, but it still hurts,” he said, pointing at the blackened blood clots on his calf.
The second part of the series is on the toll of refugee life on mental health.
*Names have been changed to protect their identity
Illustrations by Gulal Salil
We welcome feedback. Please write to respond@indiaspend.org. We reserve the right to edit responses for language and grammar.


